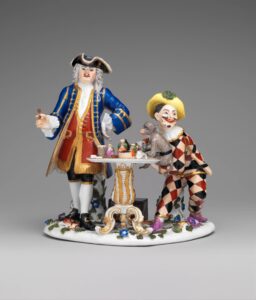
Quack doctor, harlequin and monkey. Johann Joachim Kändler for Meissen, c. 1745. Courtesy of Metropolitan Museum.
As Washington lawmakers jockeyed to repeal or eviscerate the Affordable Care Act, I was immersed in a surreal battle with my health insurance company. My experience accentuates the fact that solving the nation’s health care crisis goes far beyond turning back the latest Republican proposal.
Like so many other people who are no longer covered by a company plan, I had bought a policy through one of the state-run exchanges created by Obamacare. I chose a plan from Empire Blue Cross/Blue Shield, because most of my doctors and their affiliated hospitals accepted it. The so-called Silver plan – about mid-level in the marketplace offerings – cost more than I paid under my former employer’s plan, and the coverage wasn’t nearly as good.
Right from the start there were hassles, but nothing like what happened on the first business day of 2017. That was when my husband called our eye doctor to schedule a routine checkup and was told he had no health insurance.
“That’s impossible!” I exclaimed upon hearing the news; I had paid the $800.14 January premium well before the due date. But sure enough, when I signed onto the Empire site, our account indicated that our insurance was “suspended pending investigation.”
Pending investigation of what? I called the phone number on the back of my insurance card and waited on hold for two hours to report the problem. A customer service representative blamed it on a computer glitch.
For the next ten days, we could not make doctors’ appointments, get lab tests or fill prescriptions. “What if we have a medical emergency?” I asked, during phone calls in which I spoke to numerous people, none of whom would provide their last names or a callback number. They told me to pay any doctors we needed to see and submit the bills for reimbursement.
At the beginning of February, the same thing happened again. By then I had figured out that if I called at 7 a.m., I could get through almost immediately. Janice, in the company’s Connecticut office, suggested a second way to handle routine medical visits or even emergencies: “Have your doctor’s office call us, and we will confirm that you have coverage, even though the computer system doesn’t show it.”
I described the crowded waiting rooms and overworked staff in New York City doctors’ offices. Janice couldn’t understand how absurd it would be to burden them with that extra phone call – and why: because the IT staff at a gigantic insurance company hadn’t been able to fix a computer glitch for more than a month.
On March 1 my husband went on Medicare, so I was the only one affected when our health insurance was suspended for the third time. Now, in addition to early-morning calls to Janice, who consistently picked up at 7 a.m., I sent a Priority Mail letter to Daniel J. Tarantino, Director, Bureau of Health Insurance Programs for New York State. “I would be grateful if you would help me get my insurance reinstated and take whatever disciplinary steps against Empire you deem appropriate,” I wrote.
Not the consumer crusader I had hoped for, Tarantino delegated my crisis to his secretary, Heidi. For the next several weeks, she became my liaison to Janice in Connecticut. If I needed to reach Janice, I would first send an e-mail to Heidi, who would contact Janice, who would call me.
Wouldn’t it have been simpler to just give me Janice’s direct dial? Sure, but Empire’s protocol would not allow that.
Unfortunately, Janice couldn’t fix the problem more quickly than any of the others. But, once my insurance was reinstated, she assured me that she would keep an eye on my file and head off any future disruptions. That fell apart when Janice got the flu in early April. Fortunately, I avoided a similar malady, since my health insurance had just been suspended for the fourth time.
With no health insurance, various routine medical appointments scheduled for the following month and having exhausted all other avenues, on April 7, I sued Empire in small claims court. In my claim, for breach of contract, I sought to recover $2,763.43. That was the total in premiums paid for the months during which Empire repeatedly suspended my coverage. Though I am trained as a lawyer, it was the first case I have ever filed on behalf of myself.
Thanks to modern technology, I didn’t even need to leave the house to stand up for my rights. By using Turbocourt.com, people like me representing themselves can file court documents online. It took less than an hour to set up a Turbocourt account, fill out the one-page complaint and pay the $34.74 fee ($20 to the local small claims court and the balance for the Turbocourt service) by credit card. Several hours later I received an e-mail notifying me of my court date, on an evening ten weeks hence.
A few days after I filed the claim, Empire reinstated my insurance. It has not been suspended again. I don’t think the timing was a coincidence.
Meanwhile, I went to small claims court. I was one of about 90 people, including folks with complaints against car dealerships and contractors, who showed up at 6:30 on the appointed evening. A paralegal from Empire was there to ask for an adjournment.
Over my strenuous objection, she told the judge, Harriet L. Thompson, that we needed “to talk” about how I arrived at the $2,763.43 figure. Obviously we could have had that conversation during the two months before the court date. I showed Judge Thompson the documentation I had brought: a screenshot from my online account, taken in April, indicating that our coverage was “inactive,” and a separate screen shot, with the same date, with the premium marked “paid in full.”
Judge Thompson adjourned the case for two more months, but told the paralegal to get back to me by the end of June about a resolution. As we left the courthouse she made an offer: The company would refund the premiums, minus any claims processed during the months when our insurance was suspended. I could easily confirm that no claims had been paid.
Unfortunately, the matter didn’t end there. I had to chase the paralegal, who declined to give me her full name or e-mail address, for two more months. First, I sent a Priority Mail letter to the Empire legal department, with all my documentation attached. Simultaneously, I sent a copy of the whole package to Judge Thompson. This prompted a phone call from the paralegal, saying I needed to sign an agreement confirming the amount of the settlement. (Fine.) She promised I would be paid 30 days after returning that document.
Again, she was late. When I called and told her that she was in breach of the settlement agreement, she threatened to cancel the check she had ordered if I didn’t back off. “Do you want a check, or do you want to go back to court?” she asked rhetorically. The check finally arrived on Aug. 21, the day before our next court date.
Though I am relieved that the battle is over, it is a Pyrrhic victory. The sum I received does not make up for the time I spent or the angst I suffered – damages that one can’t fight for in small claims court. I feel sorry for other people who have been similarly mistreated by Empire and haven’t had the wherewithal to fight back.
Sadder still, my difficulties are part of a much larger crisis that’s careening toward code blue. While my case was pending, I received a notice that Empire Blue Cross/Blue Shield is leaving the New York Marketplace in 2018. And a growing number of doctors and hospitals, with their own gripes about the marketplace insurance plans, have completely stopped accepting this type of coverage. If all the major healthcare providers and insurance companies bail out, it will create a vacuum. Except for Medicare and Medicaid, there will be no one to take care of patients who can’t pay for medical expenses out of their own pockets.
Against this gloomy backdrop, the open enrollment period for 2018 health insurance will begin in November. One must choose a policy by Dec. 15 to avoid a gap in coverage. We need a system that not only provides quality health care, but also protects consumers’ rights.
Deborah L. Jacobs, a lawyer and journalist, is the author of Four Seasons in a Day: Travel, Transitions and Letting Go of the Place We Call Home and Estate Planning Smarts: A Practical, User-Friendly, Action-Oriented Guide. Follow her on Twitter at @djworking and join her on Facebook here. You can subscribe to future blog posts by using the sign-up box on her website’s homepage.
RELATED POSTS
Health Insurance for Frequent Travelers
I’m sorry to hear you went through this. The system is a mess.
Our premiums went up 72% last year for the Silver plan PPO. So, again, we had to drop to a lower quality plan that cost us more than the previous year.
Congrats on suing the snot out of them (ok, maybe it wasn’t a snot-level suit) and standing up for all of us!
The poor quality of plans is not getting nearly enough attention, and this problem is likely to get worse. What state are you in?
We’re in Illinois–so this is one of many issues that need to be addressed in the state. 🙁
I had an experience similar to yours. Bureaucratic wrangling from the get-go, as thousands of others suffered from the notorious CoverOregon. I too sought recovery of premiums I shouldn’t needed to have paid. I followed its administrative claims procedures, and after months of back-and-forth ultimately was directed to court. I too had a paralegal show up at the small claims hearing with an untimely motion to dismiss hand-delivered to me. Case postponed to allow me to respond. Showed up at court again, with yet another submission just before the hearing. Unfortunately, the court dismissed my claim …
Thank you for sharing this experience. It’s so important for consumers to speak out about what has happened. What was the court’s rationale for dismissing your claim?
I had a similar experience to yours. From the start, I faced bureaucratic issues, like many others dealing with the infamous CoverOregon. I also tried to recover premiums I shouldn’t have had to pay. After navigating the administrative claims process for months, I was eventually directed to court. At my small claims hearing, a paralegal hand-delivered an untimely motion to dismiss, causing the case to be postponed so I could respond. When I returned to court, there was yet another last-minute submission right before the hearing.